0 Reflections on the Devonport Incident and the Clothier Report of 1972
- The Steam Pulse
- by Kevin Peacock
- 06-01-2025
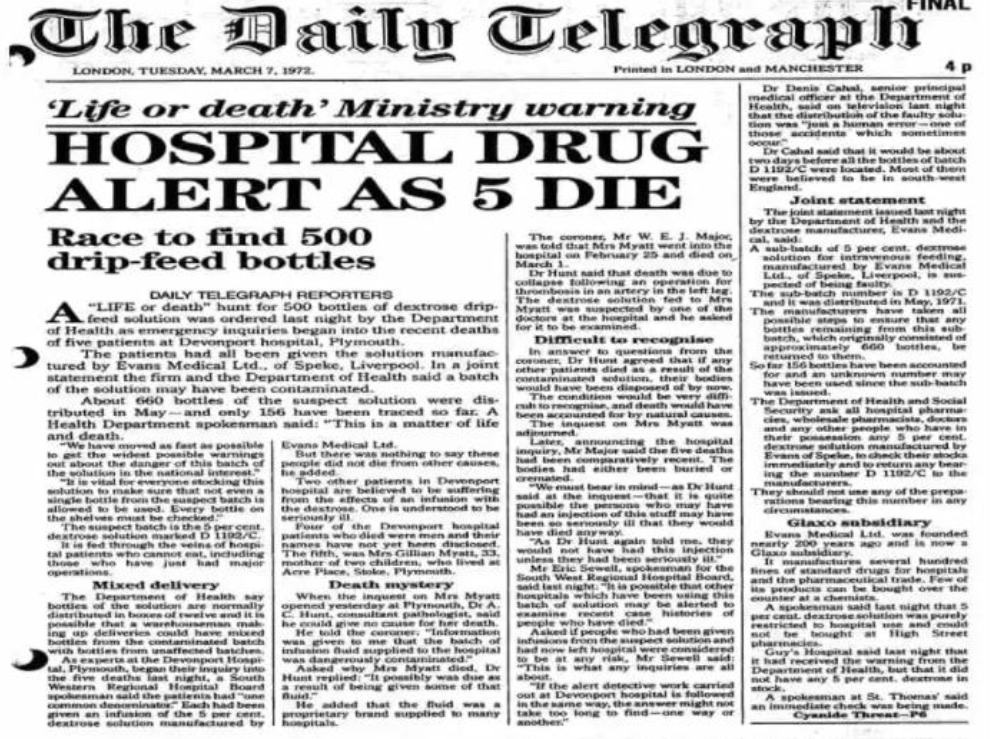
Over 50 years ago on the 12th July 1972, Dr Shirley Summerskill (MP for Halifax) spoke to the house of commons and said: -
" It is to be deplored that human failings were the main cause of the tragedy, [in March 1972] but it is hoped that all who are concerned with the preparation of infusion fluids will take a lesson from this case. I include in that remark the management and the laboratory staff."
She was of course referring to the report of the Committee which Sir Keith Joseph, Secretary of State had instructed, under the chairmanship of Mr. C. M. Clothier, QC, to inquire into the circumstances which led to the use of contaminated dextrose infusion fluids at Devonport Hospital and which involved the death of five patients.
The Committee concludes—in its own words in paragraph 79 -
" … that the fundamental cause of this disaster is to be found in human failings at Evans Medical, ranging from simple carelessness to poor management of men and plant.
The Committee heard of no imminent technological advance in the field of production of intravenous fluids which will eliminate the need for skillful men devoted to their work.
The Committee considers that too many people believe that sterilization of fluids is easily achieved with simple plant operated by men of little skill under a minimum of supervision, a view of the task which is wrong in every respect"
In 2019 David Churchward a GMP inspector for the MHRA, reflecting on the Devonport incident concluded the following -
"Despite significant progress in automation, there is still no replacement for a skilled and dedicated workforce who understand the importance of their work. Industry and regulators must maintain the highest levels of quality culture vigilance."
"MHRA inspectors look for indicators showing that personnel at all levels of the organisation have appropriate technical knowledge to enable good decision-making and understand how their actions impact the product and patient."
In his article on Quality Culture he went on to say:-
A strong quality culture is built upon:
- knowledge of what is important, and how a process achieves critical quality attributes
- diligence, by fostering awareness that everyone contributes to product quality, and understanding that “my actions impact the patient and the company”
- vigilance by individuals who know what ‘right’ and ‘wrong’ look like in their process, and a mechanism for management to be aware of problems
- senior management commitment to being visible and transparent in decision-making so that positive outcomes can be seen from the diligence and vigilance efforts. This is more than the company mission statement – it’s ‘walking the talk’”.
In the aftermath of the Clothier report being published the Medicines Inspectorate increased the number of inspectors, but they accepted that inspection alone would not be enough to prevent a recurrence. This position remains the same today as it did then.
Around the time of the incident following a history of non-sterile products in the 1960’s the role of the regional steriliser engineer was created. Charged with the responsibility for providing technical expertise and governance to the sterilisers in their charge.
This role continues today in the capacity of the Authorising Engineer (Decontamination), [AE(D)] whose role and responsibility is defined in HTM01-01 part A. [1]. They form the Decontamination Technical Platform, which constitutes registered AE(D)'s who have undergone a rigorous training framework at Eastwood Park and undergo regular peer review to ensure the high standards and expectations of IHEEM and the DTP are maintained. The DTP contributes significantly to the standards and guidance of healthcare and industry through the BSI CH198 committee for sterilization standards development; brining decades or knowledge and experience at a national and international level. [2].
In 1970 NHS Falfield (now Eastwood Park) started residential training courses for hospital engineers. This included training Test Person (Sterilisers) and the regional steriliser engineers were instrumental in the training and sharing of best practise and knowledge. This role exists today as a Competent Person (Decontamination) being defined in HTM01-01 part B, as well as the role of the Authorised Person (Decontamination), the latter responsible for the management of the decontamination and sterilisation service.[3]. Both roles are City & Guilds Accredited at Eastwood Park where AE(D)’s continue to provide robust training for hospital engineers and engineers from industry.
These roles within the Healthcare setting provide assurance that the people charged with the testing of sterilisers and their required oversight understand the fundamentals of steam sterilisation and the validation, monitoring and routine control that must be in place to provide sterility assurance. In reflection of the findings of the Clothier report 50 years ago, how confident are you in the training, competency and knowledge of the people involved in the qualification of your sterilisers and in their ongoing routine monitoring and control? Whilst the above roles are clearly defined in the UK Healthcare sector, what about Medical Devices and Pharmaceutical and how robust is your Quality Culture?
[1] IHEEM Decontamination Technical Platform - IHEEM
[2] Health Technical Memorandum 01-01. Part A: Management and provision (england.nhs.uk)
[3] Health Technical Memorandum 01-01. Part B: Common elements (england.nhs.uk)
